Work in Progress
Let's talk about Treatments (so much medical jargon coming your way so trigger warning for those skirmish)
We learn that the more you do something the easier it gets. It’s a simple fact that I’ve lived my life by. Do do do or die die die. 😉 Practising a skill makes you more equipped. It makes you more confident. It makes it easy.
Going into treatment must be the same. I am going in every month, I am going to get used to this. Every trip will be easier to get through because it will get to a point where I know the perfect way to make this effortless. That feels like a project. A challenge. And I love a challenge. I will rise to that occasion. The competitive nature will kick in and I will nail this. I’ve got this!
The most questions I get asked is about the treatments I’m receiving. How are you? How are they going? Are you feeling better?
In my head I think I put treatment equal to the word fix. A cure. A solving of a puzzle or an end to something. Some completion of a problem rather than the real description. Which is receiving medical aid for an illness. The provision, coordination or mangement of health care or services. Sometimes you have to change the way you think.
Lets get into the nitty gritty. This month we are going to really talk some medical jargon. A lot I had to look up and some I know from experience. So strap in.
I’m very thankful for my treatment and I’m very lucky to receive a drug called Tofersen.
Tofersen was developed to treat amyotrophic lateral sclerosis (ALS)/Motor Neuron Disease (MND) associated with a mutation in the superoxide dismutase 1 (SOD1) gene.
Again… just as a recap - Healthy SOD1 proteins help break down toxic byproducts produced during normal cell processes. These byproducts must be broken down regularly so they don’t damage cells. Mutations in the SOD1 gene are thought to cause the protein to misfold and clump up (aggregate) within motor neurons and astrocytes, the types of cells involved in ALS/MND development and progression. These clumps (aggregates) may interfere with healthy cell functions or may cause other necessary proteins to misfold and lose their function, damaging the nervous system and leading to the development of MND/ALS (als.org). Which is what I have.
In 2022, after an extended trial it was found to lower levels of SOD1 protein, lower levels of neurofilament light chain (a marker for nerve damage) and participants who received the drug earlier and longer - lived longer than participants who didn’t.
I’ve got this in the bag!
So how is it administered?
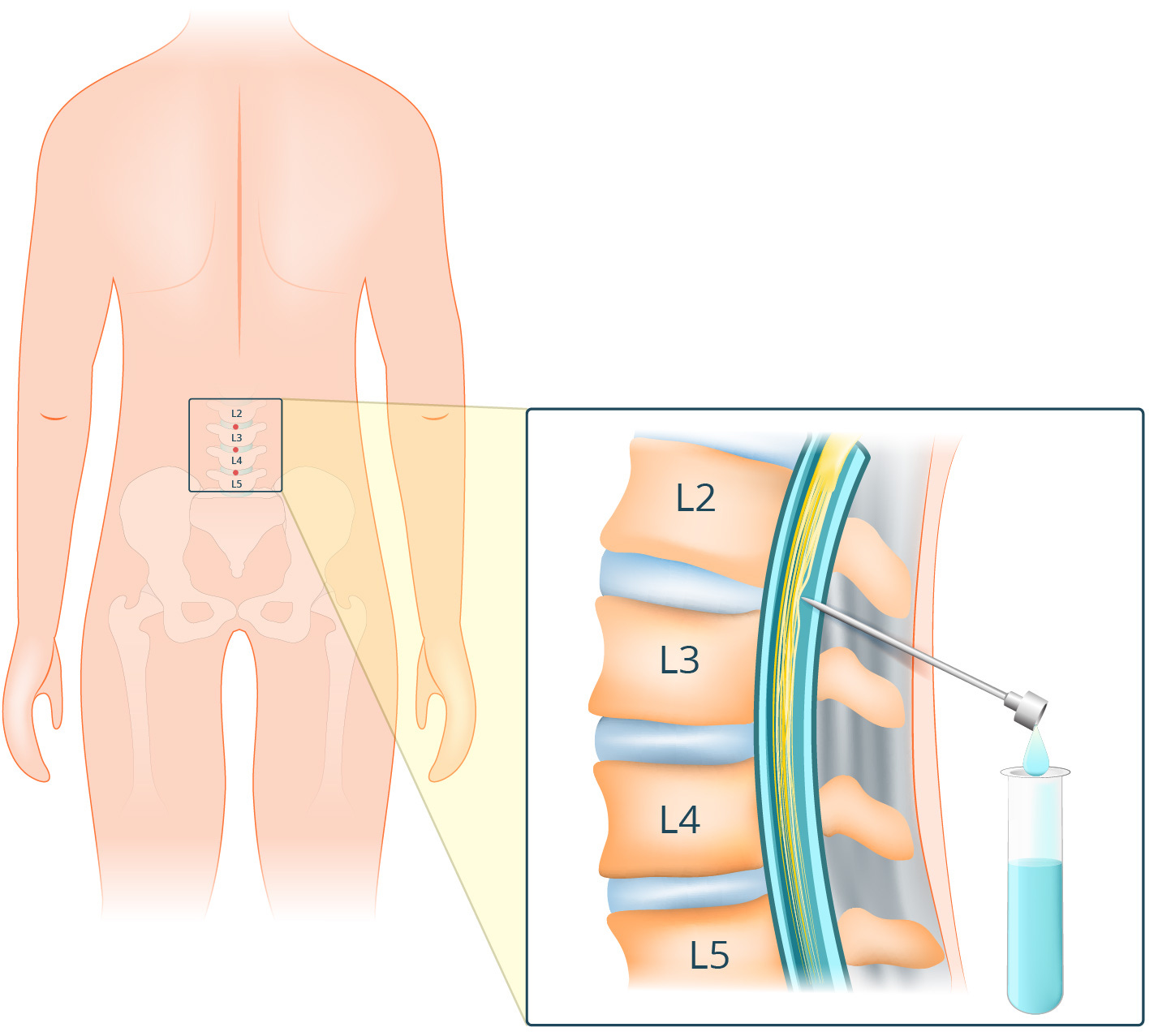
It is administered through a lumbar puncture under CT Scan. The doctor inserts a thin needle into the space around the spinal cord in the lower back and injects the drug after taking out some spinal fluid.
What is a lumbar puncture/spinal tap?
A lumbar puncture collects fluid called cerebrospinal fluid (a fluid that surrounds your brain and spinal fluid).
You get asked to lie on your side in a curled-up position or to lie on your stomach. This position helps your doctor access the space between the bones in your lower back (vertebrae). After your back is cleaned in that area, local anaesthetic will be injected into your lower back. Once the area is numb, the doctor inserts a thin, hollow needle between two bones in your lower spine. You do feel some pressure as the needle goes in.
A small amount of fluid will be collected. Once the procedure is complete, the needle will be removed and then they cover it with a bandage.
Talk me through what happens when you are there.
So now for the real talk. Generally my treatments are in the morning. I arrive 30 mins prior to ensure I’m there on time and relaxed. I’m not allowed to drive so I usually catch a cab there. Then -
Meet with the fabulous staff and take a seat inside where I have my blood pressure checked and pulse taken and go through the usual hospital sign in experience (what meds are you are on etc, what’s your details again, who are you?), take your top off and pop on a very sexy blue hospital gown.
Wait for someone from radiology to come by and go through what we are doing and run through the risks before you are asked to sign the agreement that you’re aware of all the things that could go wrong but there is only a very small percentage that is the case.
Then it’s time to go into CT Scan
The doctors and nurses change to who is on shift, so its not always the same people doing it. Of course I have my favourites. I mean who doesn’t. But you deal with who is there at the time.
The staff will usually go through how the doctor wants to deal with it today. They all have their own technique. Some prefer you on you stomach so your back is up and your feet are going in and out of the CT Scan. Others prefer you on your left side feet going in and out of the CT Scan. (this is my favourite). Another had my head going in the CT Scan and lying on my front. Hated that. I try now and talk about what I prefer. When you have had so many, you do know what works for you and what doesn’t.
Once in position, you get your blankets on or extra pillows to keep you still and you go in and out the CT Scan so they can find the easiest way to get to where they need to go. This is things like avoiding nerves etc because you don’t want to hit those! For me it’s usually quite low down the spine near the L5 and S1. Its the closest area from spine to the skin. Less distance to travel. I mean the simple thing to know is that if you are a bigger person (carrying more weight, the longer it takes to get to where they are going). Occasionally I have had it between my L4 and L5 it just depends on the doctor that day. And if its there, I’m usually lying on my stomach.
Then the area where they are going to insert the needle is cleaned and marked up with a little skirt. A little barrier they place on the back like a rectangle to keep it clean.
Now comes the local. This is the crap part. It probably is the thing that hurts the most. But only for about 40 seconds or so. Sometimes a nurse pats your hand and tells you you’re doing great. Others just let you go through it. Its a sting in the back because lets be honest a large thin needle is being driven into your back.
The doctor sitting behind you as you look to the wall away from everyone, waits for the local to take affect, to numb the area and chats with the others about what they need as the nurses prepare the utensils and doses.
Then they come back and focus on you and put a thin needle slowly into your back bit by bit. Then stop. You aren’t allowed to move. The bed slides into the CT Scan so they can see where they are going and to ensure we are on the right path. Sometimes it isn’t. So they have to pull the needle out and start again. The path needs to be clear of nerves and for some reason in my head I always thought there would be a perfect way. There is an ideal path set out we just need to find it. But it changes. It changes to how you are that day. How your back is. How the muscles are around that area that day. How the doctor is doing that day. There are so many variables that it changes each time. You’re aware of the needle and if it has go through muscle it will hurt. I’m not sure if I have a high pain threshold or not but I think I’m ok.
When they get to the point they need to go, they then insert a smaller needle within the needle and extract 10 mls of spinal fluid. The first time it happened it felt like they had tapped into my life force. I felt it in my head. And all through my body. It was an odd sensation. I haven’t had it for a long time. I do remember my headache started as soon as it was in. The doctor said, we are in your spinal fluid now and I wanted to say, I know. I could feel it. But now it changes. Sometimes I know they are in there, other times I don’t. The last time I had it done, I got a tickle in my throat when they were in there which caused a cough which mean that the needed went out of where it should be so we had to find it again. So it just depends on the day. I’ve been asked to cough before when they were at the fluid but nothing was coming out and for some reason that starts it. You start to wonder, did i have enough water today… maybe that helps. Fluid = fluid right? Who knows. Once they have their 10 mls, they take this off for testing to see how things are going.
Now it’s time for the drug itself. Usually 15 ml of Tofersen is then put into my system through the same means. If the headache hadn’t started prior it starts now. As soon as it enters my system, the headache always starts for me. It’s not huge but its about 7 on the scale of 1-10. Sharp. Annoying. I never in my life had headaches or migraines until I started on my medication. Its just a fun side effect. But I was told that i should have some coffee, or cocacola or dark chocolate to help. And also lie down obviously. So win win on those fronts. I only used to have an occasional coffee it was served in a martini glass with some vodka and kahlua. Oh boy, how things change!
Once completed with the dose, they remove the needle and pop on a bandage. A big square bandaid type seal.
When in the room (CT Scan) that procedure can take anywhere from 30 mins to 60 mins depending on how well they get into the spinal fluid. Most have been around the hour mark, but occasionally you get a lucky everything worked out fabulously and we were lucky at getting it down quickly. There is no rhyme or reason. Just a lucky day when everything aligns.
We say our thanks and then I move on to a bed on my back and get wheeled into the waiting room to rest for an hour, whilst i have my vitals checked, have chats to the nurses, eat a sandwich or crackers and check my phone alot.
Once cleared I head on out, get a pal or someone to pick me up and drive me home and we catch up for about an hour before I get on with my life or relax.
How do you feel afterwards?
It really just depends. There’s the headache for one. It happens every time. I usually have a couple of panadol and it’s all fine. When I started having them done it was when I was very busy at work so I would have treatment and then after the catch up/pick up with my pals I would go back to my desk and work and be fine. As they go on I get more fatigued. There are days that the fatigue hits early in the night and I just need to rest or go to bed early. Other times its not much at all and all it is, is feel a little tender on my lower back because of where they put the needles in. But the saying I keep saying is “its about an hour of not great for hopefully a lifetime of good”. I definitely am a bit weaker for a few days post. So I just try and relax as much as possible.
Does it get easier?
I thought it would. Practise makes perfect right? I’ve learnt that it doesn’t. It depends on how you are feeling that day. How your back is that day. Did I sleep enough last night? Am I relaxed? How late are they behind at the hospital? What the energy in the room is like? Did someone else have a bad day or evening prior. There are so many possibilities of things that are out of my control and so I just have to give over to it. I try and meditate whilst it’s happening. I say a mantra of something like “you’re ok, let the needle find it’s way to where it needs to go. You’ve got this. This is all to help. you feel stronger”. But that also takes focus and skill. To stay connected and relaxed as long needles are shoved in your back.
What I’ve learnt is what I like. I like to be calm. I like to have a warm blanket as it gets cold in the room, I like to have a pillow between my knees and under my head whilst I’m on the table. I like to know what’s going on. I need the doctors to communicate with me during the procedure so I know when we may be approaching a muscle that it may hurt as we puncture it or if there are complications and its taking longer than it should. Not knowing or having other people talk about me, for me, like i’m not present is very much not what I enjoy.
Most of the doctors have been amazing. One wasn’t. When asked to communicate with me, they said they would try. They didn’t. And so now all of them get my feedback. We work together. I am here in this room. I am present and am in that room once a month for potentially the next year and a half if not longer so let’s figure this out! Most doctors need to learn how to talk to patients or rather how to listen to them. Some are amazing - hence my favourites.
Has anything bad happened?
Not really. Althought there are a chances of things happening and definitely I have had two of those. One is the headache. That is a given every time. That’s not bad, that just feels like it should seeing they are playing with the levels of spinal fluid that go through your brain etc.
The other was a spinal fluid leak that I had one time. Normally if they know they inject blood into the site and it heals it up like an internal bandaid. However when it happened to me there was a lot going on. I was exhausted. And stressed. I had travelled back to Melbourne to have the treatment done and had fallen over at the airport. Usually when you fall over your body sends all the healing to the parts where you fell to protect it. I then had my treatment done and if it happened then my body was probably too busy helping the parts that fell that it couldn’t protect the leak that occurred.
I flew back to work a few days later and everyone i knew was sick with a flu like I had never seen, so when the whooshing sound around ears started going consistently like the feeling you were in the loudest wind tunnel you had ever walked in and the only thing was to lie down horizontal for it to stop spinning, I just thought I was getting this horrendous flu. I wasn’t. I most likely had a leak. I thought I had some inner ear infection. So that’s good to know the diference now so I can get that fixed quickly if I had to. Most of the time when you’re going through this, everything is new so you just don’t know until it happens. Which is a constant joy ;) But it has caused me to listen more to my body than I ever have before.
Is it working?
That’s a great question that I just don’t know the answer too. The studies that were done on this drug originally looked a brief period and showed no signficant difference but when they extended the study to look over two years, it showed major differences. I’m six months in. So I can’t tell you.
I feel weaker currently. My balance isn’t great anymore and although I walk with two sticks I can’t walk too far without getting exhausted. I can’t walk unassisted. I have to hold onto something in case. My left foot rolls onto the left side because the functionality to turn it flat on the ground isn’t there. The message from my brain is there its just not making its way to that spot. But we work on my balance and functionality with my trainers, physios etc.
I’m hoping to have a manual wheelchair soon to give me more access. In my head I had this real stigma against wheelchairs because I had associated them with giving up I think. But weirdly its the opposite. I took one when I was over performing in San Fran and it was a game changer. It gave me more flexibility, more ability to do things on my own terms. I wasn’t concerned about falling or not having the strength to get back to where I needed, I was safe and ok and in charge. And that was amazing.
So is it working? I’m sure it’s doing exactly what it needs to be doing which is stopping the toxicity in my body. And the less toxicity I have over time will only hopefully help my body do what it needs to do.
How many has it been?
I’m now up to number 10. I’ve had nine lumbar punctures within six months. Three the first month then one every month after that. In numerology the number 9 is powerful. It symbolizes completion of some sort. And maybe thats where we are at. The completion of a thought that no longer exists. That before - I imagined this was the golden answer to solve all my problems, that hopefully it would wipe away all my fear and anxiety but really it’s something that assists in the aid of it. It helps slowly and surely to improve the path ahead.
And for that I can only very grateful to be part of a program that can provide that.
Any questions you want me to answer? Or topics to talk about… Pop em down below. And thanks for reading.
Here’s to health and happiness